What Is The Difference Between An Anorectal Manometry Test & A Regular Manometry Test?
Anorectal Manometry Is A Term Used To Describe The Measurement Of The Size Of The Anorectal
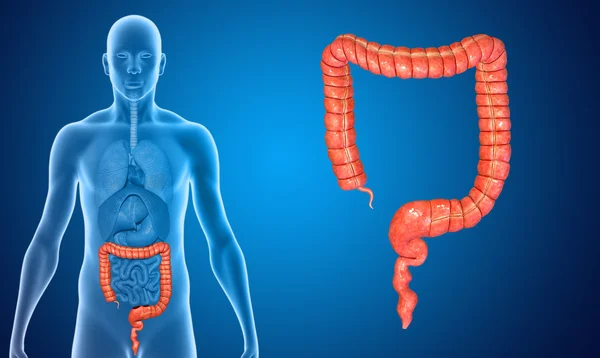
Anorectal manometry (ARM) is a bowel function test for people with fecal incontinence or persistent constipation. The approach looks at the strength of the anal sphincter muscles, feelings of feces in the rectum, bowel reflexes, and movements of the rectal and anal muscles while distending the rectum using a tiny balloon.
Anorectal manometry is a critical diagnostic technique for evaluating fecal incontinence and persistent constipation. Specialized muscles control the appropriate transit of bowel motions in the anal and rectal areas. The anal sphincter muscle normally tightens as feces reaches the rectum to avoid stool transit at an inconvenient moment. Incontinence (stool leakage) may develop if this muscle is weak or does not contract properly. Sphincter muscles can be compromised for a variety of causes, including 1) sphincter muscle tearing or partial tearing, 2) spinal cord injury, and 3) consequences from previous surgery. The anal sphincter muscles relax normally when a person pushes or bears down for a bowel movement. The pressures will drop, enabling feces to be evacuated. Constipation may be worse if the sphincter muscles contract during pushing. Anal manometry assesses the strength of the sphincter muscles and whether they relax properly during bowel movements. It helps doctors manage patients with fecal incontinence or severe constipation by providing useful information.
Electromyography of the Anal Sphincter (EMG)
Electrode Surface Small electrodes are placed peri-anally for anal EMG recording. After that, the patient is instructed to relax, squeeze, and push at various intervals. The electrical activity of the anal sphincter muscle is measured and presented on a computer screen utilizing advanced computer technology. The appropriate muscular contractions during squeezing and muscle relaxation during pushing are confirmed by EMG of the anal sphincter. During bearing down to imitate a bowel movement, the trace of electrical activity in those who constrict the sphincter and pelvic floor muscles strangely rises, rather than decreasing (defecation). A damaged sphincter muscle with normal anal EMG activity and mild anal squeeze pressures on manometry might suggest a repairable tear.
Pressure Profiling of Anorectal Rest and Squeeze
A 4-channel radial air-charged anorectal catheter will be inserted approximately 4 cm into the rectum and the patient will be positioned in a semi-recumbent position. As resting and squeeze pressures are recorded in 4 quadrants, the catheter will be gently removed at one centimeter intervals (Anterior, Right, Posterior and Left). Using modern diagnostic equipment, the average resting pressure is measured. Resting pressure should be more than 40 mmHg. Squeeze pressure will be measured on an average basis. The average squeezing pressure should be more than 100 mmHg. It is also common to measure the length of the anal canal. 3 to 4 cm is the average length of an anal canal.
Measuring Rectal Volume
The implanted rectal balloon will be progressively filled with water while the patient is in a semi-recumbent posture to assess and record the following rectal sensations: first rectal filling feeling, first desire to defecate, and maximum tolerated rectal volume. The initial feeling should be between 10 and 60 milliliters, the first desire to defecate should be between 10 and 100 milliliters, and the maximum tolerated rectal volume should be between 200 and 300 milliliters for a healthy patient.
Measurement of Rectoanal Inhibitory Reflex
The internal anal sphincter's reaction to rectal distention is the rectoanal inhibitory reflex. In the continence mechanism, the brief relaxation of the internal anal sphincter in response to rectal distention is crucial. The rectoanal inhibitory reflex will be measured when the water or air-filled catheter is inflated during the anorectal manometry test. Between 10 and 30 milliliters is what a typical response should be.
Expulsion Test using a Balloon
The balloon ejection test evaluates a patient's capacity to expel fake feces during a simulated defecation in a lab setting. A tiny balloon (as seen in Figure 1) is introduced into the rectum and filled with roughly 50 mL (2 oz) of water or air, after which the patient is requested to expel it into a toilet. The patient visits the restroom and attempts to defecate (expel) the little balloon from the rectum. The time it takes to pop the balloon is kept track of. A malfunction in the anorectal region is indicated by prolonged balloon ejection.
Summary of Procedure
It takes 30 to 45 minutes to complete the exam. A hospital gown is required for the patient. A nurse will completely explain the procedure to the patient, collect a brief medical history, lead the patient through a fecal incontinence and constipation-related health questionnaire, and answer any concerns the patient may have. After that, the patient is turned to his or her left side. The rectum is introduced using a tiny, flexible tube approximately the size of a thermometer with a balloon at the end. The electronic manometry apparatus that monitors pressure is linked to the catheter. A tiny balloon linked to the catheter may be inflated in the rectum during the test to evaluate normal reflex pathways and muscle reaction.
At different points during the procedure, the nurse will instruct the patient to relax, squeeze, or push. During each of these muscular contraction/relaxation events, the pressures in the anal sphincter are monitored. The patient squeezes the sphincter muscles as though attempting to keep anything from coming out. The patient strains down to push or bear down, as though attempting to pass gas.
As part of the whole anorectal manometry set of diagnostics, two more tests will be performed. The measurement of the time it takes to evacuate a balloon from the rectum and an anal sphincter electromyography (EMG), a test to examine the nerve supply to the anal muscle, are both explained in further detail above.
You will be able to resume your usual activities following the anorectal manometry test because it does not require anaesthetic. The physician must evaluate and understand all of the data, which takes a long time. As a result, it's possible that your doctor won't receive the test results for a few days.